FAQs
Reference
Universe Today. https://www.universetoday.com/121795/the-journey-of-light-from-the-stars-to-your-eyes/. Accessed 4/22/22.
- Optometrist or general ophthalmologist: Can perform dilated eye examinations and monitor diabetic retinopathy. Optometrists and most general ophthalmologists will refer patients who need treatment to retinal specialists. Some general ophthalmologists, who practice in rural areas or who have advanced training, will treat diabetic retinopathy with laser or injections.1
- Retinal specialist: Ophthalmology sub-specialist who treats diabetic retinopathy with laser, injections and/or surgery.
- Low vision specialist: An eye care provider (usually an optometrist) who prescribes vision aides and devices to help patients who have reduced vision complete activities of daily life.
References
- McKinney S. Debating Anti-VEGF Injections. Rev Ophthalmol. September 9, 2020. https://www.reviewofophthalmology.com/article/debating-antivegf-injections
- American Optometric Association. Eye care of the Patient with Diabetes Mellitus, second edition. 2019. https://www.aoa.org/AOA/Documents/Practice Management/Clinical Guidelines/EBO Guidelines/Eye Care of the Patient with Diabetes Mellitus, Second Edition.pdf
All URLs accessed 4/17/22.
References
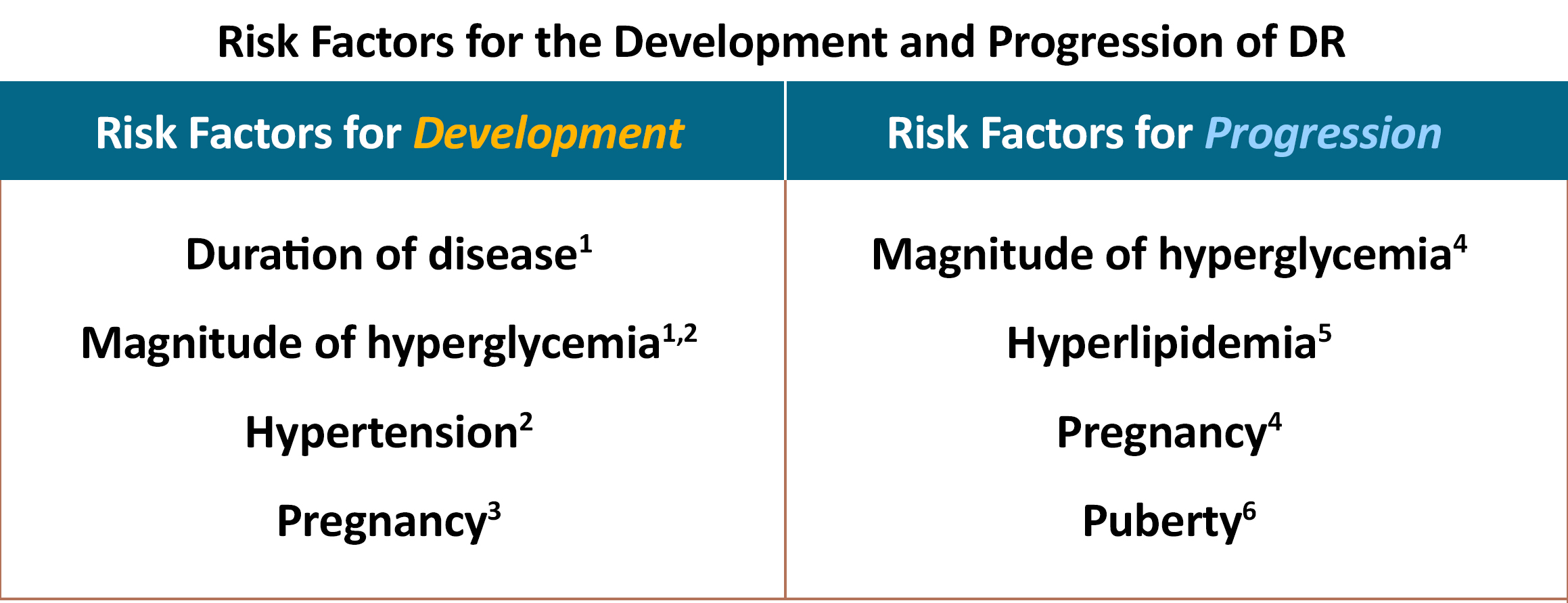
- Ferris FL 3rd, Nathan DM. Editorial. Preventing Diabetic Retinopathy Progression. Ophthalmology. 2016;123:1840-1842.
- Xie X, Atkins E, Lv J, et al. Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis. Lancet. 2016;387(10017):435-443.
- Chew EY, Mills JL, Metzger BE, et al. Metabolic control and progression of retinopathy. The Diabetes in Early Pregnancy Study. National Institute of Child Health and Human Development Diabetes in Early Pregnancy Study. Diabetes Care. 1995;18(5):631-637.
- Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. The Diabetes Control and Complications Trial Research Group. Diabetes Care. 2000;23(8):1084-1091.
- Shi R, Zhao L, Wang F, et al. Effects of lipid-lowering agents on diabetic retinopathy: A Meta-analysis and systematic review. Int J Ophthalmol. 2018;11(2):287-295.
- Lueder GT, Silverstein J. American Academy of Pediatrics Section on Ophthalmology and Section on Endocrinology. Screening for retinopathy in the pediatric patient with type 1 diabetes mellitus. Pediatrics. 2005;116(1):270-273.
- Panretinal photocoagulation (PRP): A laser is used to make many small burns in the retina to reduce the likelihood of neovascularization of the retina.1
- Focal Laser: A laser used to make one or a few small burns in the retina to treat damaged blood vessels.2
- Anti-VEGF medication: This medication is injected into the eye to prevent blood vessels from leaking and prevent neovascularization.3 It is also used to decrease swelling from diabetic macular edema (DME).4
- Corticosteroid medication: This medication is injected into the eye to reduce inflammation and swelling in the retina.5
- Vitrectomy: A surgical treatment option for eyes with persistent vitreous hemorrhage (bleeding in the gel like tissue in front of the retina) or eyes with persistent disease despite medical, laser and injection treatment.5
References
- The Diabetic Retinopathy Study Group. Indications for photocoagulation treatments of diabetic retinopathy: Diabetic Retinopathy Study Report no. 14. Int Ophthalmology Clin. 1987;27(4):239-253.
- Early Treatment Diabetic Retinopathy Study Research Group. Treatment techniques and clinic guidelines for photocoagulation of diabetic macular edema. ETDRS study report number 2. Ophthalmology. 1987;94:761-774.
- Writing Committee for the Diabetic Retinopathy Clinic Research Network. Panretinal photocoagulation vs intravitreous ranibizumab for proliferative diabetic retinopathy: A randomized clinic trial. JAMA. 2015;314:2137-2146.
- Mitchell P, Bandello F, Schmidt Erfurth U, et al. The RESTORE study: ranibizumab monotherapy or combined with laser versus laser monotherapy for diabetic macular edema. Ophthalmology. 2011;188:615-625.
- Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020;127(1):P66-P145.
References
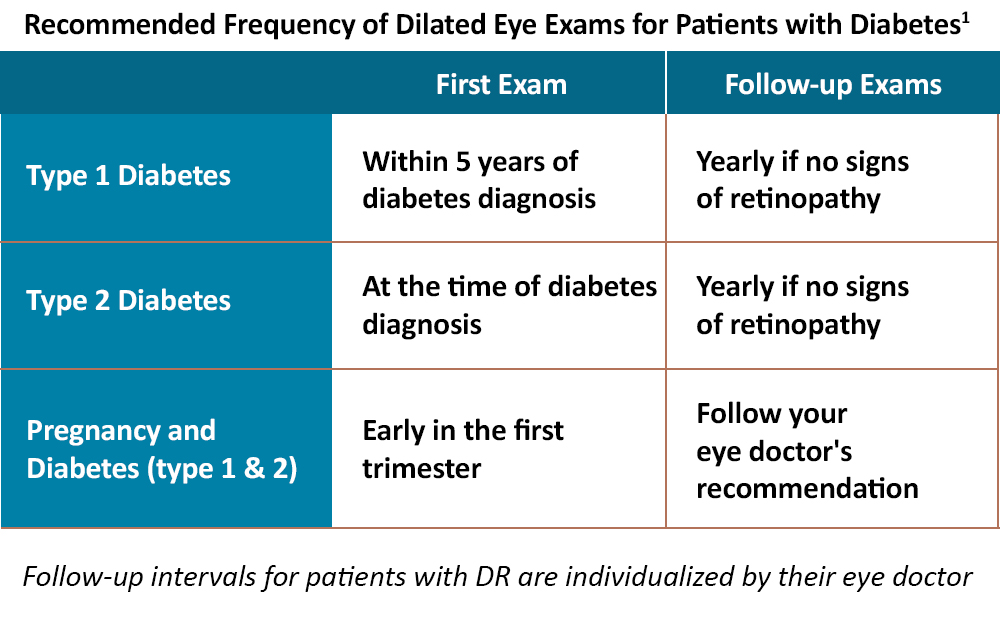
- 1. Flaxel CJ, Adelman RA, Bailey ST, et al. Diabetic Retinopathy Preferred Practice Pattern®. Ophthalmology. 2020;127(1):P66-P145.
- Myth: Excellent eyesight (having 20/20 vision) is correlated with excellent eye health.
Fact: It is possible to have diabetic retinopathy (DR) without any symptoms. Early detection of DR is vital. The better the vision is prior to treatment, the better the vision will be after treatment.1 - Myth: Patients with diabetes are receiving the recommended dilated eye examinations.
Fact: Referral for dilated eye examination is provided for <50% of diabetic patients seen by primary care and <86% seen by endocrinology.2,3 - Myth: Diabetic retinopathy (DR) is the only complication of diabetes present in the eye.
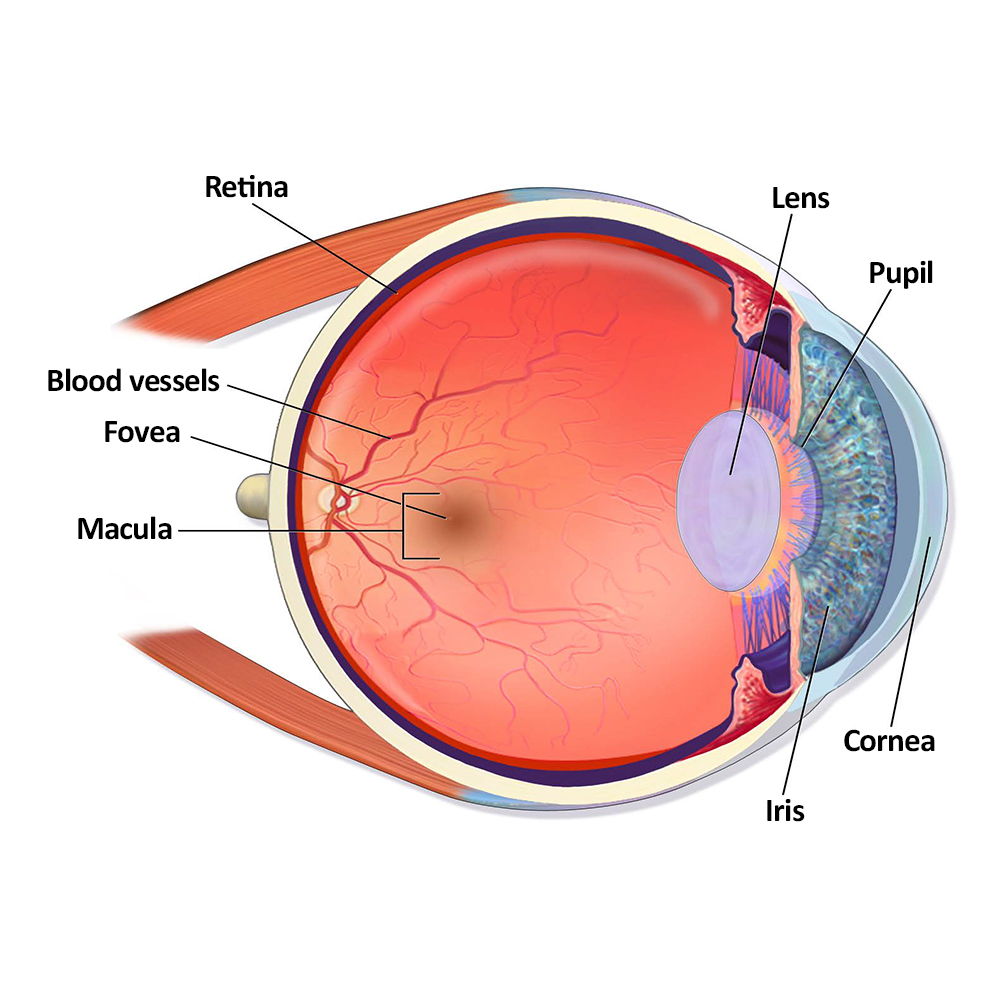
Fact: Diabetes can affect the eye in many ways beyond DR. The non-retinal effects include changes in visual acuity (20/20, etc), color vision, ability to focus on near objects (accommodation), changes in the visual field (peripheral vision), loss of contrast sensitivity (ability to detect subtle differences in shade and pattern), nerve palsies that effect muscles that move the eye, changes in pupil reactions, microaneurysms on the conjunctiva (white tissue on the front of the eye), dry eyes, slower healing from wounds, changes in the color of the iris, higher risk for glaucoma, cataracts and increased risk of neuropathy of the optic nerves.4 - Myth: A patient who has well controlled diabetes will not develop DR.
Fact: In patients with diabetes, there is no glycemic threshold when the risk of DR is eliminated.5
References
- Sophie R, Lu N, Campochiaro PA. Predictors of functional and anatomical outcomes in patients with diabetic macular edema treated with ranibizumab. Ophthalmology. 2015;122(7):1395-1401.
- Kraft SK, Marrero DG, Lazaridis EN, et al. Primary care physicians’ practice patterns and diabetic retinopathy: current levels of care. Arch Fam Med. 1997;6(1):29-37.
- Silva FQ, Adhi M, Wai KM, et al. Evaluation and Referral of Diabetic Eye Disease in the Endocrinology and Primary Care Office Settings. Ophthalmic Surg Lasers Imaging Retina. 2016;47(10):930-934.
- American Optometric Association. Eye care of the Patient with Diabetes Mellitus, second edition. 2019. Accessed 4/17/22. https://www.aoa.org/AOA/Documents/Practice Management/Clinical Guidelines/EBO Guidelines/Eye Care of the Patient with Diabetes Mellitus, Second Edition.pdf
- Diabetes Control and Complications Trial Research Group. Effect of pregnancy on microvascular complications in the diabetes control and complications trial. Diabetes Care. 2000;23(8):1084-1091.